Radiotherapy efficacies for vertebral hemangioma patients with severe spinal cord compression and cauda equina syndrome—case report and literature review
Highlight box
Key findings
• Conventional radiotherapy could improve neurological symptoms for patients with inoperable vertebral hemangioma.
What is known and what is new?
• Radiotherapy is an effective alternative treatment of pain relief for patients with inoperable vertebral hemangioma.
• Our case reports showed that two patients with vertebral canal encroachment by hemangioma, accompanied by neurologic deficits, experienced complete regression of neurologic symptoms after completion of radiotherapy with 42–44 Gy in conventional fractions.
What is the implication, and what should change now?
• Radiotherapy could provide clinical benefits for patients with hemangioma-associated vertebral canal encroachment and accompanying neurological deficits.
Introduction
Vertebral hemangiomas are the most common benign spinal tumors, with a prevalence rate of approximately 12%. They are enriched with blood-filled cavities and mostly occur in the thoracic and lumbar spine (1,2). Vertebral hemangioma, which causes thickened vertebral trabeculae, is classically characterized by polka dot and corduroy signs on radiographic computed tomography (CT) scans (3). On magnetic resonance imaging (MRI), vertebral hemangiomas often manifest as hyperintense signals in which the signal values are dependent on the composition of adipocytes, edematous tissue, and vascularity of the vertebral hemangioma (4).
Although vertebral hemangiomas are benign tumors, some patients develop spinal cord compression accompanied by pain symptoms and subsequent neurological deficits (1,5). Surgery remains the mainstay of treatment for these patients. However, for patients with comorbidities who are ineligible for surgery, treatment options are limited. Herein, we present two cases of inoperable aggressive vertebral hemangioma with prominent spinal cord compression causing severe neurological deficits in accordance with the CARE reporting checklist (available at https://tro.amegroups.com/article/view/10.21037/tro-23-8/rc). The patients responded to radiotherapy and fully recovered from their neurological symptoms.
Case presentation
Patient 1
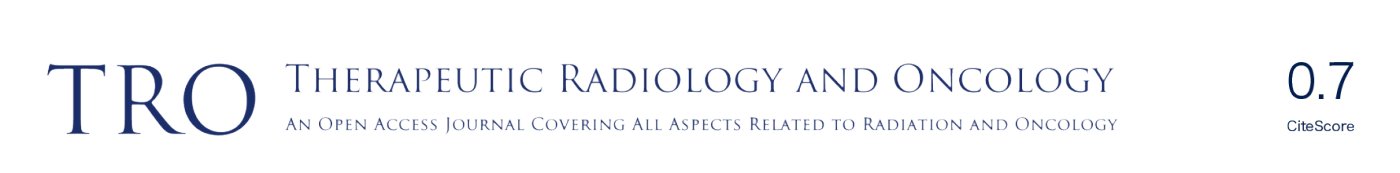
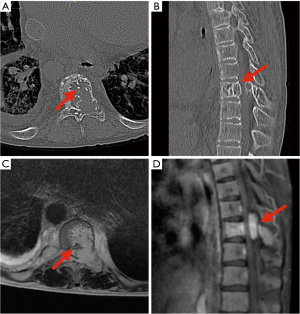
A 17-year-old boy presented with dysesthesia of the right foot and an unsteady gait that had persisted for one month. Later, he experienced progressive dysesthesia and bilateral weakness in bilateral lower extremities. Neurological examination revealed that his Medical Research Council’s scale (MRC scale) for muscle power was four out of five. As symptoms progressed (MRC scale muscle power: 3), the patient became wheelchair-dependent for ordinary daily living activities. The CT scan showed polka dot and corduroy signs at the ninth thoracic vertebra (T9) (Figure 1A,1B). MRI revealed a T2-weighted hyperintensity and gadolinium-enhanced T1-weighted hypointensity, with an expansile lesion at T9 which caused spinal cord compression (Figure 1C,1D). Based on these classical radiographic findings, the patient was diagnosed with vertebral hemangioma at T9. The patient was unsuitable for surgery due to a cyanotic heart defect and therefore underwent radiotherapy at 44 Gy in 20 fractions using helical tomotherapy and concurrent administration of dexamethasone (Figure 2).
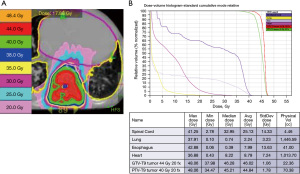
Upon completion of radiotherapy, the patient’s bilateral lower-limb dysesthesia subjectively improved without treatment-related adverse toxicities. At 5.5 months after the completion of radiotherapy, he fully recovered from neurological symptoms (MRC scale muscle power of the lower extremities returned to five) and returned to normal activities of daily living. Follow-up MRI also showed partial regression of the vertebral hemangioma at T9. The patient remained neurologically deficit-free 34 months after the completion of radiotherapy, and MRI revealed almost complete remission of the T9 vertebral hemangioma (Figure 3).
Patient 2
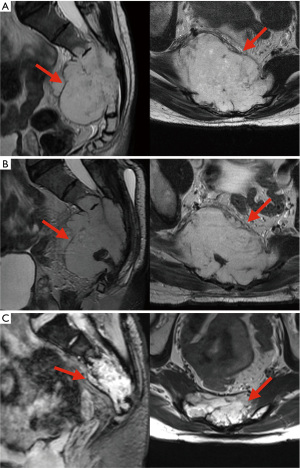
A 36-year-old man initially complained of right buttock numbness for five months. Subsequently, he experienced right leg pain and numbness, accompanied by difficulty with defecation. MRI revealed a T2-weighted hyperintensity and gadolinium-enhanced T1-weighted lesion in the sacrum, which caused cortical destruction and total sacral nerve root encasement (Figure 4A). Pathology of the sacral tumor biopsy specimen revealed a hemangioma, confirming sacral hemangioma with cauda equina syndrome. The patient underwent transcatheter arterial embolization (TAE), but his symptoms persisted, with a slightly enlarged tumor after TAE (Figure 4B). Hence, the patient underwent radiotherapy for the sacral hemangioma with 42 Gy in 21 fractions, using volumetric modulated arc therapy (VMAT). During radiotherapy, the patient experienced subjective improvement in right leg pain and numbness. Soon after the completion of radiotherapy, he experienced subjective improvement in difficulty with defecation. Grade 1 or 2 dermatitis and fatigue were observed during and after radiotherapy. Six months after the completion of radiotherapy, the patient showed complete recovery of neurological symptoms, including pain, numbness, and difficulty with defecation. Follow-up MRI revealed partial remission of the hemangioma 2 years after completing radiotherapy and good partial remission of the sacral lesion eight years after the completion of radiotherapy (Figure 4C).
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the Helsinki declaration (revised version in 2013). Written informed consent was obtained from patient 1’s parents and patient 2 for publication of their cases and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
In addition to surgery, previous studies have reported that radiotherapy may serve as an alternative treatment option for vertebral hemangioma (6-14). Rades et al. analyzed 117 patients with vertebral hemangioma and categorized them into high-radiotherapy dose (36–44 Gy) and low-radiotherapy dose (20–34 Gy) groups according to the equivalent dose in 2 Gy per fraction (EQD2), in which an α/β ratio of 3 was applied because vertebral hemangioma is a low-proliferative benign disease (6). Rades et al. reported that patients in the high-dose radiotherapy group achieved better symptom control (up to 82%) without experiencing an increase in toxicity (6). Heyd et al. recruited 84 patients with symptomatic vertebral hemangioma (82 patients with pain and 24 patients with spinal cord compression accompanied by paresis of neurological symptoms) and showed that radiotherapy with a median dose of 34 Gy (range, 4.5–45 Gy) provided an overall response rate of 90% in pain relief [complete response (CR), 52 (61.9%); partial response (PR), 24 (28.6%)] (7). Regarding neurological symptom relief (n=20), the authors reported that radiotherapy resulted in an overall response rate of 100% (CR, 79.2%; PR, 20.8%). However, in their study, 20 patients underwent surgical intervention before radiotherapy. It is unclear whether most patients with neurological symptoms underwent initial surgical intervention. In addition, using multiple logistic regression analyses, the authors showed that radiotherapy >34 Gy provided better pain relief than radiotherapy <34 Gy. Furthermore, Heyd et al. reviewed the literature on radiotherapy for symptomatic vertebral hemangiomas and reported that radiotherapy resulted in a CR rate of 57.6% (n=200) and PR rate of 27.7% (n=96) for pain relief in a total of 347 cases from 64 published studies (7). A similar radiation dose schedule was also endorsed by two large retrospective studies (8,9) in which the radiotherapy dose was at least 36 Gy in 2 Gy per fraction, which could offer feasible treatment outcomes for patients with vertebral hemangioma, with complete pain relief ranging from 59% to 64% (Table 1).
Table 1
| Series (institution) (Ref) | N | RT (Gy) | Complete pain relief | Neurological deficits improvement | Notes |
|---|---|---|---|---|---|
| University Hospital Eppendorf (6) | ≥36 Gy resulted in better pain relief | ||||
| Group A | 62 | 20–34 (2 Gy/fx) | 39% | NA | |
| Group B | 55 | 36–44 (2 Gy/fx) | 82% | NA | |
| Multicenter German Study (7) | 84 | 4.5–45 (median 34 Gy/17 fx) | 62% | CR =79%; PR =21% | ≥34 Gy resulted in better pain relief |
| Maria Sklodowska-Curie Center (8) | 137 | 8–30 (81% 24 Gy/12 fx) | 64% at 1.5 years | NA | Increase RT dose and fx size resulted in better pain relief |
| Akdeniz University Hospital (9) | 80 | 30–40 (median 40 Gy/20 fx) | 59% | NA | Patients with concomitant musculoskeletal disease had lower pain relief |
| University of Florida (10) | 10 | 28.8–59.8 (median 45 Gy/25 fx) | NA | NA | 90% local tumor control at 30 years |
| National Cancer Database (11) | 56 | Mean: 19.36 | NA | NA | Overall survival: >35 vs. 0–35 Gy; at 50 months: 21% vs. 0%, P=0.0073 |
| Peking University Third Hospital (13) | 20 | 40–50 (20–25 fx) | NA | CR =65% | VCE >40% resulted in poor RT response |
| Maria Sklodowska-Curie Center randomized trial (14) | Exclude patient with hemangioma-related neurological symptoms; CK arm result in better pain relief | ||||
| CK arm | 38 | 25 (5 fx) | 73.7% | NA | |
| Conventional arm | 36 | 36 (18 fx) | 50% | NA | |
RT, radiotherapy; fx, fraction; NA, non-analysis; CR, complete response; PR, partial response; VCE, vertebral canal encroachment; CK, CyberKnife.
In a follow-up study of 10 patients with symptomatic vertebral hemangioma over 5 years, Parekh et al. showed that radiotherapy with a mean dose of 47 Gy provided a 90% tumor control rate and recommended a favored radiotherapy dose of 45 Gy in a 1.8 Gy per fraction schedule for treating vertebral hemangioma (10). In an analysis of the National Cancer Database, searching for hemangiomas between 2004 and 2016, Patel et al. identified 102 patients with histologically proven spinal hemangiomas who underwent different treatments, including surgical approaches, chemotherapy, and radiotherapy (11). Patel et al. further showed that, among 56 patients receiving radiotherapy, a higher dose of radiotherapy (>35 Gy) was significantly associated with better overall survival (at 25 months, 37.5% vs. 10%, P=0.0073) (11). The aforementioned results should be interpreted with caution because the endpoints thereof primarily focused on pain relief but did not specifically describe improvements in neurological deficits, and some patients also underwent surgical intervention before radiotherapy (Table 1).
Another case series conducted by Jiang et al. analyzed the treatment outcomes of 29 patients with vertebral hemangioma who had neurological deficits (12), of whom 2 of the 10 patients who received radiotherapy alone required further surgical intervention for progressive neurological deficits. However, the radiotherapy dose was not mentioned in this report (12). Wang et al. assessed the clinical outcomes of 20 patients with vertebral hemangioma who had mild neurological deficits (defined as MRC scale for muscle power of greater than three out of five) and were treated with radiotherapy using 40–50 Gy in 20–25 fractions. In their study, 13 patients (65%) achieved complete resolution of neurological symptoms without recurrence after a minimum follow-up of 20 months (Table 1) (13). Moreover, among those receiving radiotherapy with 40 to 50 Gy, seven patients who experienced progressive or stable neurological symptoms after radiotherapy had more severe vertebral canal encroachment (greater than 40% at initial MRI examination), whereas 13 patients who responded to radiotherapy had an encroachment ratio less than 40% (Table 1) (13). In contrast, our first presented case had a spinal canal encroachment of 63.4% and was completely free of neurological symptoms 5.5 months after completing radiotherapy. The other patient had complete encroachment (100%) of the sacral plexus by the sacral hemangioma and achieved good partial remission of the tumor, with complete recovery from difficult defecation, leg pain, and numbness after completing radiotherapy.
Miszczyk et al. conducted a randomized controlled trial that focused on two different radiotherapy schedules for relieving pain at two years in patients presenting with painful vertebral hemangiomas. This randomized trial excluded patients who exhibited hemangioma-related neurological deficits or pain caused by cord compression (14). A total of 74 patients were randomly assigned to two treatment arms: the CyberKnife (CK) arm (25 Gy in 5 fractions using CK) and the conventional arm (36 Gy in 18 fractions using a linear accelerator). When compared to patients in the conventional arm, more patients in CK arm experienced improvement in pain (at 2 years, 73.7% vs. 50%, P=0.036), but the percentage of decreased numerical rating scale (NRS) and adverse effects were not significantly different between CK and conventional arms (NRS: 67% vs. 50%, P=0.407) (Table 1) (14). Although this trial did not enroll patients with vertebral hemangioma with neurological deficits, the hypofractionated radiotherapy regimen provided more subjective pain relief than the conventional radiotherapy regimen. This trial also provided the information that the hypofractionated regimen is likely to substitute the conventional regimen, and most importantly, shorter and more intensive course of radiotherapy could be beneficial for patients with acute neurological deficits. Further exploration of the efficacy of relieving neurological deficits caused by vertebral hemangiomas using hypofractionated radiotherapy regimens (such as 25 Gy in 5 fractions) is warranted.
Wang et al. retrospectively analyzed the clinical outcomes of 39 patients with vertebral hemangiomas who presented with neurological deficits or spinal cord compression (Enneking stage 3, S3) and were required to undergo decompression with (n=22) or without (n=17) intraoperative vertebroplasty (15). In their study, postoperative radiotherapy of 40–50 Gy was administered to patients who had a residual vertebral lesion on the 3-month postoperative follow-up images. None of the 22 patients who underwent decompression plus intraoperative vertebroplasty (18 patients without radiotherapy) experienced recurrence. Of the 17 patients who underwent decompression, one of nine patients without radiotherapy developed recurrence and underwent decompression followed by adjuvant radiotherapy. At a median follow-up of 50.2 months (range, 13–134 months), none of the patients had vertebral hemangioma recurrence (15). Wang et al. also reviewed the literature regarding the association between different surgical approaches, including decompression surgery, intralesional vertebrectomy, and total en bloc spondylectomy, and clinical outcomes for aggressive vertebral hemangioma (at least Enneking stage 3). Their results showed that the aforementioned surgical approaches provided the optimal control rate for aggressive vertebral hemangioma (15). In another retrospective study of 21 patients with aggressive vertebral hemangioma (all with neurologic deficits) who underwent different surgical procedures, including intralesional spondylectomy with reconstruction (n=9), stabilization, decompression, and vertebroplasty (n=9), and decompression and stabilization (n=3), all patients experienced improvement of neurological symptoms; only one patient developed a local recurrence at a mean follow-up of 55.78 months (range, 24–96 months) (16). Considering that the technique of decompression surgery is relatively undemanding and that several studies have shown that vertebroplasty or radiotherapy may prevent local recurrence (15,17,18), decompression surgery and intraoperative vertebroplasty followed by radiotherapy for residual lesions is recommended for patients with aggressive vertebral hemangioma without comorbidities.
There are few reports describing clinical outcomes and management of vertebral hemangioma from Taiwan. Hwang et al. reported that a 55-year-old woman who presented with a mono paresis of the left leg resulting from a T10 vertebral hemangioma, and this patient had neurologic symptoms-free at 6 months after undergoing a T10 laminectomy but without postoperative radiotherapy (19). In the retrospective analyses of 184 patients who underwent surgical approaches for intraspinal tumors, Wu et al. showed that the most common histological subtype was Schwannoma (55 cases, 54%), while only 3 patients (3%) of them were histologically proven to be hemangioma (20). In this study, we reported two patients who could not undergo surgical approaches but well responded to the conventional dose of radiotherapy. Although these are the first two case reports of vertebral hemangioma treated by radiotherapy in Taiwan, further studies exploring the treatment efficacies of conventional or hypofractionated radiotherapy alone for Taiwanese patients with inoperable vertebral hemangioma are warranted.
Conclusions
Our study, together with those reported in the literature, demonstrated that radiotherapy with a conventional dose of at least 40 Gy resulted in significant improvements in neurological symptoms. The use of radiotherapy can be an alternative treatment strategy for patients with inoperable vertebral hemangioma, even if the disease manifests as severe spinal cord compression accompanied by neurological deficits.
Acknowledgments
Funding: This work was supported by the National Taiwan University Hospital, Taiwan (NTUH 112-S0215).
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://tro.amegroups.com/article/view/10.21037/tro-23-8/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tro.amegroups.com/article/view/10.21037/tro-23-8/coif). S.H.K. serves as an unpaid Associate Editor-in-Chief of Therapeutic Radiology and Oncology. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the Helsinki declaration (revised version in 2013). Written informed consent was obtained from patient 1’s parents and patient 2 for publication of their cases and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gaudino S, Martucci M, Colantonio R, et al. A systematic approach to vertebral hemangioma. Skeletal Radiol 2015;44:25-36. [Crossref] [PubMed]
- Slon V, Stein D, Cohen H, et al. Vertebral hemangiomas: their demographical characteristics, location along the spine and position within the vertebral body. Eur Spine J 2015;24:2189-95. [Crossref] [PubMed]
- Rodallec MH, Feydy A, Larousserie F, et al. Diagnostic imaging of solitary tumors of the spine: what to do and say. Radiographics 2008;28:1019-41. [Crossref] [PubMed]
- Baudrez V, Galant C, Vande Berg BC. Benign vertebral hemangioma: MR-histological correlation. Skeletal Radiol 2001;30:442-6. [Crossref] [PubMed]
- Dang L, Liu C, Yang SM, et al. Aggressive vertebral hemangioma of the thoracic spine without typical radiological appearance. Eur Spine J 2012;21:1994-9. [Crossref] [PubMed]
- Rades D, Bajrovic A, Alberti W, et al. Is there a dose-effect relationship for the treatment of symptomatic vertebral hemangioma? Int J Radiat Oncol Biol Phys 2003;55:178-81. [Crossref] [PubMed]
- Heyd R, Seegenschmiedt MH, Rades D, et al. Radiotherapy for symptomatic vertebral hemangiomas: results of a multicenter study and literature review. Int J Radiat Oncol Biol Phys 2010;77:217-25. [Crossref] [PubMed]
- Miszczyk L, Tukiendorf A. Radiotherapy of painful vertebral hemangiomas: the single center retrospective analysis of 137 cases. Int J Radiat Oncol Biol Phys 2012;82:e173-80. [Crossref] [PubMed]
- Aksoy RA, Aksu MG, Korcum AF, et al. Radiotherapy for vertebral hemangioma: the single-center experience of 80 patients. Strahlenther Onkol 2022;198:648-53. [Crossref] [PubMed]
- Parekh AD, Amdur RJ, Mendenhall WM, et al. Long-term Tumor Control With Radiotherapy for Symptomatic Hemangioma of a Vertebral Body. Spine (Phila Pa 1976) 2019;44:E731-4. [Crossref] [PubMed]
- Patel S, Ansari D, Patil SN, et al. High-Grade Spinal Hemangioma: A National Cancer Database Analysis. World Neurosurg 2021;148:e527-35. [Crossref] [PubMed]
- Jiang L, Liu XG, Yuan HS, et al. Diagnosis and treatment of vertebral hemangiomas with neurologic deficit: a report of 29 cases and literature review. Spine J 2014;14:944-54. [Crossref] [PubMed]
- Wang B, Meng N, Zhuang H, et al. The Role of Radiotherapy and Surgery in the Management of Aggressive Vertebral Hemangioma: A Retrospective Study of 20 Patients. Med Sci Monit 2018;24:6840-50. [Crossref] [PubMed]
- Miszczyk M, Napieralska A, Woźniak G, et al. Conventionally fractionated radiotherapy versus CyberKnife hypofractionated radiotherapy for painful vertebral haemangiomas - A randomized clinical trial. Radiother Oncol 2022;176:46-52. [Crossref] [PubMed]
- Wang B, Han SB, Jiang L, et al. Intraoperative vertebroplasty during surgical decompression and instrumentation for aggressive vertebral hemangiomas: a retrospective study of 39 patients and review of the literature. Spine J 2018;18:1128-35. [Crossref] [PubMed]
- K GP, Shetty AP, K S SVA, et al. In Vertebral Hemangiomas with Neurological Deficit, Is a Less Extensive Approach Adequate. Asian Spine J 2023;17:37-46.
- Templin CR, Stambough JB, Stambough JL. Acute spinal cord compression caused by vertebral hemangioma. Spine J 2004;4:595-600. [Crossref] [PubMed]
- Goldstein CL, Varga PP, Gokaslan ZL, et al. Spinal hemangiomas: results of surgical management for local recurrence and mortality in a multicenter study. Spine (Phila Pa 1976) 2015;40:656-64. [Crossref] [PubMed]
- Hwang SL, Wu CH, Chen YT, et al. Monoparesis of the leg caused by thoracic vertebral hemangioma: a case report. Neurol Sci 2012;33:709-10. [Crossref] [PubMed]
- Wu YL, Chang CY, Hsu SS, et al. Intraspinal tumors: analysis of 184 patients treated surgically. J Chin Med Assoc 2014;77:626-9. [Crossref] [PubMed]
Cite this article as: Chen PJ, Chen YL, Yang SH, Kuo SH. Radiotherapy efficacies for vertebral hemangioma patients with severe spinal cord compression and cauda equina syndrome—case report and literature review. Ther Radiol Oncol 2023;7:25.