Brain injury from an unexpected source: a case report
Highlight box
Key findings
• Embolic sources in patients with ischemic stroke caused by intracardiac masses.
What is known and What is new?
• Primary cardiac tumors are rarely found to cause an embolic disease, therefore its known less than 5% of all cardiac tumors.
• This manuscript showed the differential diagnosis of embolic sources caused by intracardiac masses.
What is the implication, and what should change now?
• Cardiac magnetic resonance imaging may be considered to exclude the differential diagnosis of other intracardiac masses, such as cardiac lipomas.
• In patients with atypical features, preoperative biopsy and confirmation are essential to evaluate the prognosis and guide treatment.
Introduction
Background
Primary cardiac tumors are rarely found, therefore its known less than 5% of all cardiac tumors. Benign tumors amount to more than 75% of primary heart tumors, of which myxomas (50%) are the most common, followed by papillary blastoma (20%), lipoma (15–20%), and hemangiomas (5%) (1). Neurological complications can be the beginning complication of a cardiac tumor likely around 80% of cases. Embolization or thrombi of tumor develop in up to 45% of patients, half of which are associated with the central nervous system.
Rationale and knowledge gap
The most common complication of cardiac tumors is neurological manifestation can be understood as a sequence of the late onset. Patients with ischemic stroke are usually hospitalized during active embolization of heart tumors (2). Cardiac magnetic resonance (CMR) becomes a main protagonist for diagnose and differentiate various type of intracardiac masses.
Objective
This case report aims to improve the knowledge of the differential diagnosis of embolic sources caused by intracardiac masses. We present this article in accordance with the CARE reporting checklist (available at https://tro.amegroups.com/article/view/10.21037/tro-23-19/rc).
Case presentation
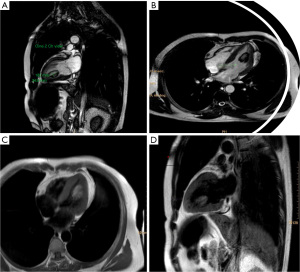
A 46-year-old male with history no cardiovascular risk factor like hypertension, smoker, or diabetes mellitus. While the patient was at home, he started to feel right-sided weakness and dysarthria. He was rushed by ambulance to a local hospital. A stroke team was deployed. A computed tomography (CT) of the head showed no acute embolic stroke. From initial examination, his vital sign, physical examination, and electrocardiogram (ECG) within normal limit. ECG showed sinus rhythm with heart rate (HR) 95 beats per minutes, frontal axis normal, horizontal axis normal, P wave 0.05 s, QRS complex 0.04 s, no ST-T changes. His transthoracic echocardiogram disclosed a highly mobile lobular mass of 18.2 mm × 34.2 mm, attached to mid-wall of the left ventricle (LV). Systolic function and the LV wall motion were normal. After initial examination conducted at the local hospital, he was admitted to Premiere Hospital Surabaya to obtain further examination. The differential diagnoses that were considered enclosed by LV mass or thrombus. Tissue characterization was conducted using CMR. CMR demonstrated a non-enhancing non-pedunculated mobile 18.2 mm × 34.2 mm mass (Figure 1), within the LV mid wall and anterolateral papillary muscle. This mass appeared bright on T1-weighted fast spin-echo magnetic resonance imaging (MRI) and hypointense on T1-weighted fat suppressed sequences. On T2-weighted short-inversion-time inversion-recovery (STIR) typically used to null the signal from fat, additive T1 + T2 contrast. All these findings were diagnostic for a benign cardiac lipoma and can be treated with surgery. Surgery was concluded through a median sternotomy with cardiopulmonary bypass. A left atriotomy method become no longer capable of detected the stalk of the mass, so a left ventriculostomy become completed and the mass become removed, due to the fact the mass connected to anterolateral papillary muscle, so we determined to take away papillary muscle additionally update the valve with mechanical valve Advancing The Standart (ATS) No. 29. From histopathology examination, we found muscular mass consist of lipid form. The affected person had a monotonous post-surgical course and become discharged home. There was no adverse event in this case. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Publication of this case report and accompanying images was waived from patient consent according to the Faculty of Medicine, Brawijaya University institutional review board.
Discussion
Cardiac lipoma is an uncommon benign primary cardiac tumor showed for the number of 2–8% of all benign cardiac tumors (3). The typical “recommended age” for patients are 40 to 60 years, but referrals can occur at any age and no gender predilection (4). Occasionally, they are asymptomatic and often disclosed by coincidence. Symptoms for cardiac lipoma are diverse, depends on the part of the heart. Benign tumors in the sub pericardium can produce mass effects on adjacent structures. The tumor may cause angina if they press the coronary arteries, or the LV and the systolic function will by decrease. Myocardial tumors can infiltrate the electrical circuit and be the focal point of arrhythmias. Therefore, the most frequent localization is the sub myocardial region, with a specific projection for the right atrium and LV. Depending on the cavity involved and the size of the mass, they can cause outflow obstruction and congestive heart failure. Embolism is a rare occurrence because lipomas are often encapsulated (5,6).
The initial diagnosis is usually established by echocardiography. CT scan and cardiac MRI are usually subsequently performed and may help elucidate the nature of the tissue (i.e., lipomatous tissue) and extent of infiltration (7). On CMR examination, homogeneous appearance of lipomas has an escalated signal intensity on T1-weighted imaging, with a reduction in signal intensity in fat-saturated sequences (6,8). In the other hand, with the administration of intravenous contrast even cardiac lipomas do not show an enhance intensity. Other embolic sources that can be a differential diagnosis for this case is rhabdomyoma. The MRI characteristic for this tumor was hypodense mass in T1 and homogeneously hyperdense in T2. There was no clear distinction found between its edge and the inferior ventricular wall. This characteristic was slightly similar with cardiac lipoma, but it can be differentiated by knowing the patient profile. Usually rhabdomyoma referred to early age, whilst in cardiac lipoma occurred on older age (9). However, in some cases, cardiac imaging could miss some points to confirm the diagnosis, therefore a surgical excision and histopathologic examination is required.
However, there is a consensus that said surgical resection of all cardiac lipomas, regardless of symptoms or obstruction, is generally pursued by numerous reports in the literature on the associated risks of sudden cardiac death. Cardiac lipomas are easy to resect as they are encapsulated and rarely invade the myocardium cardiac lipomas are encapsulated and rarely invade the heart muscle, making them easy to remove. If the excision is done early, the lipoma is small, and LV function is maintained, the surgical risk is low. Possible complications of lipectomy include left ventricular contractile dysfunction, ventricular septal defect, and ventricular arrhythmia (10). Deaths have also been addressed after resection of a very large left ventricular lipoma in a patient with preoperative left ventricular systolic dysfunction (1). In some special case, the patient died within 2 weeks of surgery, caused by heart failure and refractory ventricular fibrillation. The diagnosis of cardiac lipomas can be concluded on postoperative pathological examination that showed mature fat cells and fibrous membrane (6).
Conclusions
Cardiac lipoma is a rare benign heart tumor. They are well characterized in cardiac MRI. However, in patients with atypical features, preoperative biopsy and confirmation are essential to evaluate the prognosis and guide treatment.
Acknowledgments
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://tro.amegroups.com/article/view/10.21037/tro-23-19/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tro.amegroups.com/article/view/10.21037/tro-23-19/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Publication of this case report and accompanying images was waived from patient consent according to the Faculty of Medicine, Brawijaya University institutional review board.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Shamsi F, Bajwa G, Ghalib H. "Left ventricular lipoma…. a rare case", case report. J Cardiothorac Surg 2020;15:85. [Crossref] [PubMed]
- Hrdlicka CM, Wang J, Selim M. Neurological Complications of Cardiac Procedures. Semin Neurol 2021;41:398-410. [Crossref] [PubMed]
- Rocha RV, Butany J, Cusimano RJ. Adipose tumors of the heart. J Card Surg 2018;33:432-7. [Crossref] [PubMed]
- D'Souza J, Shah R, Abbass A, et al. Invasive Cardiac Lipoma: a case report and review of literature. BMC Cardiovasc Disord 2017;17:28. [Crossref] [PubMed]
- Motwani M, Kidambi A, Herzog BA, et al. MR imaging of cardiac tumors and masses: a review of methods and clinical applications. Radiology 2013;268:26-43. [Crossref] [PubMed]
- Wang Y, Wang X, Xiao Y. Surgical treatment of primary cardiac valve tumor: early and late results in eight patients. J Cardiothorac Surg 2016;11:31. [Crossref] [PubMed]
- Arslan S, Gundogdu F, Acikel M, et al. Asymptomatic cardiac lipoma originating from the interventricular septum diagnosed by multi-slice computed tomography. Int J Cardiovasc Imaging 2007;23:277-9. [Crossref] [PubMed]
- Bajaj RR, Deva D, Kirpalani A, et al. Cardiac magnetic resonance imaging for non-invasive diagnosis of lipomatous hypertrophy of inter-atrial septum. Indian Heart J 2014;66:244-6. [Crossref] [PubMed]
- Bassareo PP, Fanos V, Tavera MC, et al. Left ventricular giant rhabdomyoma in an infant with no tuberous sclerosis: accidental finding and complex management. Turk J Pediatr 2010;52:420-2. [PubMed]
- Sun X, Liu G, Kim H, et al. Left ventricular lipoma resected using thoracoscope-assisted limited sternotomy: A case report and literature review. Medicine (Baltimore) 2018;97:e11436. [Crossref] [PubMed]
Cite this article as: Handari S, Hazzy F, Paramitha AD. Brain injury from an unexpected source: a case report. Ther Radiol Oncol 2023;7:24.