The third irradiation to a recurrent nasopharyngeal carcinoma with magnetic resonance-guided stereotactic body radiation therapy: a case report
Highlight box
Key findings
• This case report depicts a pioneering experience of using magnetic resonance-guided (MR-guided) stereotactic body radiation therapy (SBRT) for the third irradiation to the repeatedly loco-regional failures of nasopharyngeal carcinoma (NPC) in Taiwan.
What is known and what is new?
• The third irradiation is rarely seen under the consideration of probably higher incidence and severity of fatal toxicities.
• The combination of MR-guided Linear Accelerator and SBRT minimizes the possibility of fatal events in this case.
What is the implication, and what should change now?
• For repeatedly loco-regional recurrences of NPC, MR-guided SBRT may reduce unnecessary doses to the organs at risk around the planning target volume.
Introduction
Nasopharyngeal cancer (NPC) is relatively rare worldwide, with an age-standardized rate below 1 per 100,000 person-years (1). More than 70 percent of new cases are found in East and Southeast Asia, with the Middle East and North Africa being the second most common areas (2). In Taiwan, according to the 2019 Taiwan Cancer Registry Annual Report, NPC was ranked as the 12th most common malignancy in the male population and 20th in the female population (3). The age-standardized rate for men was 7.48 per 100,000 person-years, and 2.02 per 100,000 person-years for women, while the mean diagnosed age for both genders was 52 years (3).
Due to the high sensitivity to ionizing radiation, radiotherapy is the main treatment modality for early NPC, while concurrent chemoradiotherapy remains the standard regimen for locoregionally advanced patients (4). Nevertheless, even after completion of the whole treatment course, 10% of this population still has residual or recurrent disease (5). Salvage surgery, systemic therapy, or radiotherapy are the main treatment options, while surgery is for resectable disease, and systemic therapy and/or radiotherapy is suggested for remaining cases (6). While applying radiotherapy to residual or recurrent disease, cautiously administered treatment is advised, since there is a concern of fatal radiation toxicity impacting neighboring normal organs (7).
The authors demonstrate the first case receiving the third irradiation course using magnetic resonance-guided (MR-guided) stereotactic body radiation therapy (SBRT) in Taiwan for repeatedly loco-regional recurrences of NPC. We present this case in accordance with the CARE reporting checklist (available at https://tro.amegroups.com/article/view/10.21037/tro-22-38/rc).
Case presentation
In December, 2010, a 31-year-old woman visited our hospital, complaining of suffering from a stuffy left ear for over 3 weeks. After examination, this was determined to be nonkeratinizing carcinoma, undifferentiated, over bilateral nasopharynx, with invasion to sphenoid bone and sinus. An enlarged lymph node (1.99 cm in diameter) was located at the left retropharyngeal space, while bilateral neck level II lymphadenopathy were also noted under positron emission tomography-computed tomography (PET-CT). According to the American Joint Committee on Cancer 7th edition of cancer staging, she was diagnosed with NPC, cT3N2M0, stage III. Induction chemotherapy followed by concurrent chemoradiotherapy was administered with total irradiation dose of 70 Gray in 35 fractions (70 Gy/35 Fr), five times per week daily using Tomotherapy. Complete remission was shown by computed tomography (CT) 3 months later. She was then placed under integrative and regular follow-up at three departments in our hospital: Otorhinolaryngology Department, Hematology and Oncology Department, and Radiation Oncology Department, with nasopharyngoscopy and magnetic resonance imaging (MRI) being conducted every three months, and with yearly PET-CT.
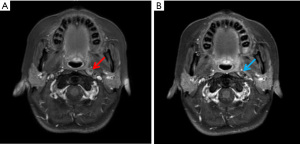
Four years later, the routine MRI showed left retropharyngeal lymphadenopathy. After discussion between the patient and the interprofessional collaborative team, a second irradiation course for this patient was planned with conventional fractionation using Tomotherapy. Total dosage of 60 Gy in 30 fractions (60 Gy/30 Fr) was delivered to the recurrent left retropharyngeal nodes, scheduled five times per week (Figure 1), and adjuvant chemotherapy was also performed. From that time, she was placed under surveillance at multidisciplinary outpatient departments with regular imaging and fiberscope follow-up. Stable disease of the recurrent retropharyngeal nodes was maintained (Figure 2).
Unfortunately, intolerable symptoms manifested in June, 2021, with this being 11 years after her first diagnosis of NPC and 7 years after the second irradiation course. These included left neck stiffness and intermittent left parietal headache, and owing to the gradually bulging left retropharyngeal region, difficulty in swallowing also developed leading to choking as the most bothersome condition. PET-CT showed naso-oropharnyngeal region invasion with temporal styloid process involvement and encasement of the internal carotid artery. The image findings seemed compatible with all of the reported symptoms. Considered as an unresectable disease, intravenous chemotherapy was initially suggested by the medical team, but the patient sought help from radiotherapy due to refusal to undergo this process.
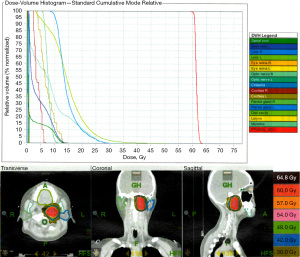
It was challenging to administer the third irradiation course alone to the same failure site, as the repeatedly recurrent cancer cells were much more radio-resistant after the initial two courses of irradiation. As a result, the treatment method was cautiously designed with MR-guided SBRT, combining the precision of MR-guided imaging per day and sharp-dose concentration of SBRT, with the aim being to deliver radiation doses to the target volume centralized with minimal influence on nearby critical organs. The high-risk possibility of iatrogenic radiotherapy-related morbidity and mortality such as carotid artery blow-out was fully discussed with the patient, who fully understood such irretrievable risk and decided to go ahead with the third irradiation course. SBRT with total dose of 35 Gy in 5 fractions (35 Gy/5 Fr) was administered on an alternate day schedule in June, 2021 (Figure 3). Grade 1 mucositis was noticed during treatment, with no other acute side effects.

Subsequently, the symptoms of posterior neck stiffness and headache gradually subsided, while the choking episodes almost disappeared. Three months later, MRI showed shrinkage of the metastatic lymphadenopathy in the radiation field. The latest yearly PET-CT on May 23rd, 2022 showed partial treatment response (8) (Figure 4). Interval-reduced fluorodeoxyglucose (FDG) with avid swollen tissues and avid residual focal FDG in the roof of the mouth [maximum standardized uptake value (SUVm): 2.2] and eustachian tube (SUVm: 5.6) were found. The latest outpatient department visit was one year after the third irradiation (in July, 2022), with the patient seeming well without possible sickness or complications shown. The palliative effect and freedom from acute toxicity were maintained for at least 1 year after MR-guided SBRT. For future toxicity observation, further outpatient close monitoring at Hematology and Oncology departments monthly, and at the Radiation Oncology department every two months will be performed.

All procedures performed in this study were in accordance with the ethical standards of the Institutional and/or National Research Committee(s) and with the Helsinki Declaration (as revised in 2013). Written inform consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Discussion
Among NPC patients with loco-regional recurrences, 41% are detected within the first 2 years, and 44% in the second to fifth year (1). The mean time from the diagnosis of primary NPC to the detection of loco-regional recurrence is approximately 30 months (9). Over 96% of recurrences occur in the previous high-dose irradiation zone (9). In contrast, marginal failures are relatively uncommon (9). For local-regionally recurrent NPC, salvage treatment options include surgery, re-irradiation, and systemic therapy. However, there is no data of randomized controlled trial to compare the three treatment methods so far, although some retrospective studies have indicated that patients with lower disease volume or earlier recurrent T-staging were eligible surgical candidates for salvage surgery (10). On the contrary, surgery is not recommended if the recurrent tumor volume involves the lateral wall of the sphenoid sinus, cavernous sinus, intracranial invasion, or skull base (10). For unresectable recurrences, radiotherapy with intensity-modulated radiation therapy (IMRT) is the most used modality at present. A conventional radiation dose over 60 Gy to the recurrent gross tumor volume (rGTV) is advised, with this threshold of 60 Gy achieving a local control rate approaching 52–86% (11).
Beside conventional fractionation, a SBRT regimen of 24–48 Gy in six fractions for re-irradiation to recurrent NPC has been mentioned as another radiotherapy choice (12). Total dose of 24–45 Gy in 3–5 fractions has also been reported, with a 5-year overall-survival rate of 60% and a loco-regionally failure-free survival rate of 79% (12). The time interval between each irradiation course has been suggested to be over 2 years (13). Some protocols recommend that while using SBRT as re-irradiation, the maximum cumulative dose should be less than 125 Gy of equivalent total doses in 2-Gy fractions (EQD2) (13).
Based on previous studies, there are three aspects associated with the biological benefit of SBRT. First, the CHISEL trial had shown that a reduced overall treatment time might conquer the repopulation of tumor cells (14). Second, a larger dose size improves the lack of re-oxygenation in chronically hypoxic tumor cells, inducing further tumor cell killing (14). Third, a larger dose size also causes vascular endothelial cell damage, leading to indirect tumor cell death (15).
The characteristics of radiation physics of SBRT are also beneficial. If 70–80% prescription dose line is planned to cover more than 95% of the planning target volume (PTV), the non-uniform peak dose will distributes in the center of the PTV (16). So the dose fall-off is relatively faster around the PTV and the doses to neighboring normal organs will be much lower (14).
Clinicians should be aware of fatal complications arising from the re-irradiation to loco-regionally recurrent NPC, with the most common toxicities including carotid blowout, temporal lobe necrosis, and mucosal necrosis (7). Consequences include massive hemorrhage, radiation encephalopathy, and dysphagia (7). A recent meta-analysis expressed that grade 5 toxicities could be realized in 33% of the re-irradiation populations (17).
For this patient, we planned a SBRT regimen using the first MR-guided linear accelerator (MR-Linac) in Taiwan at our department. MR-Linac has the capability of visualization of soft-tissue features for more precise target volume delineation (8). It is also available to proceed with online adaptive dose distribution for each fraction if necessary (18). Based on the much clearer soft tissue details than CT-image-guided, the combination of MR-Linac and SBRT technique has offered a new way to minimize the expansion margins and the overlaps between target volume and organs at risk (19). It avoids unnecessary doses to the organs at risk around nasopharynx.
Look back on the three irradiation courses that this patient has gone through (70 Gy/35 Fr, 60 Gy/30 Fr, and 35 Gy/5 Fr), the irradiation intervals were 4 years and 7 years respectively. The cumulative dose was 179.58 Gy (EQD2) in total (70 Gy plus 60 Gy plus 49.58 Gy, while 49.58 Gy was the EQD2 of 35 Gy/5 Fr SBRT under α/β ratio of 10). After the third irradiation for symptom palliation using SBRT in June, 2021, the patient has already had better quality of life for over 1 year without signs of carotid blowout, temporal lobe necrosis, mucosal necrosis, massive hemorrhage or radiation encephalopathy. However, there are scarcely any reports discussing the third irradiation to the loco-regional failures of NPC. Longer and intensive follow-up under close surveillance for this patient is definitely required.
In the long run, this lady was firstly diagnosed of NPC shortly after giving birth to her first baby at the age of 31 years old. What motivated her to survive was the vital desire to participate in her baby’s growing up. Since the first diagnosis of NPC, she has already lived over 11 years and her life is still going on.
Conclusions
This case report depicts the first experience of using MR-guided SBRT for the third irradiation to repeatedly regional recurrences of NPC in Taiwan. It also brings three points prospectively. Firstly, the biology benefits, radiation physics, efficacy and precision of the third irradiation using SBRT on MR-Linac are accomplishable. Secondly, the palliative effect and tolerable acute toxicity are achieved. Finally, patient-centered care and shared decision-making between the medical team and the patient are both indispensable on the long road to the conquest of cancer.
Acknowledgments
We thank all the members of the Department of Radiation Oncology of Kaohsiung Medical University Hospital for their support. We thank Mr. Tredrea Stephen Russell of KIWI Communicative Language Enterprises Incorporation, Kaohsiung, Taiwan for English editing.
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://tro.amegroups.com/article/view/10.21037/tro-22-38/rc
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://tro.amegroups.com/article/view/10.21037/tro-22-38/coif). C.J.H. serves as an unpaid editorial board member of Therapeutic Radiology and Oncology from May 2022 to April 2024. The other authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the Institutional and/or National Research Committee(s) and with the Helsinki Declaration (as revised in 2013). Written inform consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Au KH, Ngan RKC, Ng AWY, et al. Treatment outcomes of nasopharyngeal carcinoma in modern era after intensity modulated radiotherapy (IMRT) in Hong Kong: A report of 3328 patients (HKNPCSG 1301 study). Oral Oncol 2018;77:16-21. [Crossref] [PubMed]
- Ferlay J, Colombet M, Soerjomataram I, et al. Cancer statistics for the year 2020: An overview. Int J Cancer 2021; Epub ahead of print. [Crossref] [PubMed]
- 2019 Taiwan Cancer Registry Annual Report. In: Administration THP, editor. 2022.
- Pow EH, Kwong DL, McMillan AS, et al. Xerostomia and quality of life after intensity-modulated radiotherapy vs. conventional radiotherapy for early-stage nasopharyngeal carcinoma: initial report on a randomized controlled clinical trial. Int J Radiat Oncol Biol Phys 2006;66:981-91. [Crossref] [PubMed]
- Ye W, Chang ET, Liu Z, et al. Development of a population-based cancer case-control study in southern china. Oncotarget 2017;8:87073-85. [Crossref] [PubMed]
- Liu YP, Li H, You R, et al. Surgery for isolated regional failure in nasopharyngeal carcinoma after radiation: Selective or comprehensive neck dissection. Laryngoscope 2019;129:387-95. [Crossref] [PubMed]
- Chen J, Dassarath M, Yin Z, et al. Radiation induced temporal lobe necrosis in patients with nasopharyngeal carcinoma: a review of new avenues in its management. Radiat Oncol 2011;6:128. [Crossref] [PubMed]
- de Leon J, Woods A, Twentyman T, et al. Analysis of data to Advance Personalised Therapy with MR-Linac (ADAPT-MRL). Clin Transl Radiat Oncol 2021;31:64-70. [Crossref] [PubMed]
- Li JX, Huang SM, Jiang XH, et al. Local failure patterns for patients with nasopharyngeal carcinoma after intensity-modulated radiotherapy. Radiat Oncol 2014;9:87. [Crossref] [PubMed]
- Chan JYW, Wong STS, Wei WI. Surgical salvage of recurrent T3 nasopharyngeal carcinoma: Prognostic significance of clivus, maxillary, temporal and sphenoid bone invasion. Oral Oncol 2019;91:85-91. [Crossref] [PubMed]
- Tian YM, Zhao C, Guo Y, et al. Effect of total dose and fraction size on survival of patients with locally recurrent nasopharyngeal carcinoma treated with intensity-modulated radiotherapy: a phase 2, single-center, randomized controlled trial. Cancer 2014;120:3502-9. [Crossref] [PubMed]
- Nam H, Ahn YC, Yang K, et al. Re-irradiation with Moderate Hypo-fractionation Using Intensity Modulated Photon or Proton Radiation Therapy in Locally Recurrent Squamous Cell Carcinoma of Nasopharynx. Cancer Res Treat 2022;54:96-108. [Crossref] [PubMed]
- Liu S, Lu T, Zhao C, et al. Temporal lobe injury after re-irradiation of locally recurrent nasopharyngeal carcinoma using intensity modulated radiotherapy: clinical characteristics and prognostic factors. J Neurooncol 2014;119:421-8. [Crossref] [PubMed]
- Brand DH, Kirby AM, Yarnold JR, et al. How Low Can You Go? The Radiobiology of Hypofractionation. Clin Oncol (R Coll Radiol) 2022;34:280-7. [Crossref] [PubMed]
- Brown JM, Carlson DJ, Brenner DJ. The tumor radiobiology of SRS and SBRT: are more than the 5 Rs involved? Int J Radiat Oncol Biol Phys 2014;88:254-62. [Crossref] [PubMed]
- Nahum AE. The radiobiology of hypofractionation. Clin Oncol (R Coll Radiol) 2015;27:260-9. [Crossref] [PubMed]
- Lee NY, Zhang Q, Pfister DG, et al. Addition of bevacizumab to standard chemoradiation for locoregionally advanced nasopharyngeal carcinoma (RTOG 0615): a phase 2 multi-institutional trial. Lancet Oncol 2012;13:172-80. [Crossref] [PubMed]
- Hall WA, Paulson E, Li XA, et al. Magnetic resonance linear accelerator technology and adaptive radiation therapy: An overview for clinicians. CA Cancer J Clin 2022;72:34-56. [Crossref] [PubMed]
- Randall JW, Rammohan N, Das IJ, et al. Towards Accurate and Precise Image-Guided Radiotherapy: Clinical Applications of the MR-Linac. J Clin Med 2022;11:4044. [Crossref] [PubMed]
Cite this article as: Weng YY, Chen F, Huang CJ. The third irradiation to a recurrent nasopharyngeal carcinoma with magnetic resonance-guided stereotactic body radiation therapy: a case report. Ther Radiol Oncol 2023;7:22.